“I long to empower aspiring wounded healers to first heal themselves and to revitalize the nearly-lost art of psychotherapy – empowering seekers to become their best selves and be more vitally alive individuals; I know from colleagues I am not alone with this desire.” ~ Pam Chubbuck
Revitalization of the Nearly-Lost Art of Depth Psychotherapy Needed: An Antidote to Psychiatric Medication Madness © May 2014
by Pamela Chubbuck, PhD, LICSW, LPC
Two cases in recent months of what I call “medication madness” prompted some in-depth study. Cases that could have been handled well, with better immediate outcomes, if the clients had had access to quality depth psychotherapy. We need more psychotherapists trained in how to help clients with the expression and processing of strong feelings, including having done their own deep work so that they are not afraid of deep feelings. Theirs or their clients.
These cases compelled me to research, which yielded alarming, little-known facts* about psychiatric medications. Some of you are probably more aware than I was of these facts. Psychiatrist Peter Breggin, MD first wrote about “Medication Madness” in his book by the same name in 2008. Atlanta-based psychiatrist Charles Whitfield, MD and numerous other psychiatrists and psychologists around the world have also written over the last two decades about the ill effects of psychiatric medications.
(*All below is supported by hard scientific evidence, many published papers (including peer-reviewed) and books, FDA archived information and legal cases where pharmaceutical companies misled the public, caused harm to many and were ordered to pay damages. Case information is not factually altered other than for confidentiality of identities.)
Frequently colleagues send out inquiries, seeking psychiatrists for medication referrals. I was fortunate to have years of training by three psychiatrists who did not prescribe medications; instead they worked with the childhood, and other trauma, long held within, to allow a person to heal.
I have made a long career of trying my best to assist people to live well medication-free, for numerous reasons, primarily past client reports and desires. And my experience, and receiving client feedback over 30 years, that medication made it more difficult at best, to process the emotions necessary for their healing. Read below, cases exploring this difficulty.
Case 1: Ten years ago, Angie consulted me after 4 emergency room admissions for abdominal pain. Nothing had been found wrong medically. Some physicians thought Angie was “making this up”, but had no suggestions about how to heal other than psychiatric medications. Referred to me by a friend – during our first hour together we discovered the root of the problem and began to move the energy that had been stuck in her bodymind for 20 years. Her sister had died when Angie was 14 and upon receiving the news Angie collapsed on the floor and started crying loudly. A doctor was summoned. Angie was immediately put on tranquilizing medications for several weeks. Her sister’s death was never discussed. Two years later Angie’s mother died. This time Angie had well learned to suppress all her feelings and the same dynamics occurred – no one processed Mom’s death. Ever. Now at age 34 Angie’s bodymind could no longer hold the emotions; what emerged was the prior somatization of her deep grief compounded by anger that no one had allowed her to express her feelings.
Clearly, it is not helpful to medicate someone experiencing deep emotions – feelings that need to be expressed. This is often done because the family and/or therapist cannot tolerate deep emotions – theirs or others. Angie did wonderfully with supportive skills to express, process and integrate her repressed emotions. After 3 sessions her physical symptoms abated, never to return in these years she has stayed in touch with me.
 “Recommending medication in a crisis in effect says to the patient, ‘You and I cannot handle this. We need to do something to your brain.’ Instead of growing through the crisis, the person succumbs to the crisis. A great opportunity for learning and self-transformation is wasted.”
“Recommending medication in a crisis in effect says to the patient, ‘You and I cannot handle this. We need to do something to your brain.’ Instead of growing through the crisis, the person succumbs to the crisis. A great opportunity for learning and self-transformation is wasted.”
~ Psychiatrist, Peter R. Breggin MD
The dramatic increase of medications routinely suggested or prescribed in recent years is profoundly disturbing. Our country seems to have gone mad about psychiatric drugs. Consumers, therapists, physicians and drug companies have all become “mad” – in the old meaning of the word – that is – “not always sane, grounded, realistic” – about taking, suggesting or prescribing psychiatric medications.
Regarding over-prescribing of medication, psychiatrist Charles Whitfield, MD wrote, “When the only tool you have in your toolbox is a hammer, everything looks like a nail.”
We too often passively accept huge drug company campaigns to sell the idea to patients, prescribers, psychiatrists and psychotherapists alike, that their products are the answers to problems and will “cure” people of life’s hard issues.
Cymbalta and other drugs are advertised on TV prime time, and we laugh off the lengthy lists of side effects, which are not really side effects at all but actually effects. Drug companies are certainly mad, but also cunning – they know what they are doing – making money – and risking many people’s health by altering brain chemistry (cashing in on misinformation about “chemical imbalances” and arguments such as “Just like a diabetic needs insulin…” is all clever fraud**). Millions of children are being diagnosed with ADHD and prescribed stimulant drugs such as Ritalin when the efficacy, safety, and long-term effects of such drugs are now seriously in doubt.
We all know the tobacco industry deceived the American public for decades causing horrific damage and deaths to tens of thousands of people. Recently in the news has been Toyota’s negligence regarding a problem with one model of their cars that became a death-trap. No surprise then, that Big Pharma sells us propaganda that psychiatric drugs are safe and effective, all the while concealing hard evidence to the contrary, including burying information about “unsuccessful” drug trials. All in pursuit of money.
Case 2: A mother contacted me, desperate for help – her 20 year old daughter was hospitalized after attempting suicide. The mother felt the hospital was not providing effective help and a friend of hers recommended a Psycho-Spiritual Personal Intensive with me. Her daughter Jessica, a junior in college, had swallowed her entire Cymbalta supply and some thumb tacks, and then went to the hospital; where she later made a second “attempt”. Jessica had a history of multiple brain surgeries for a benign brain tumor starting at age 12. The surgeries left her partially, permanently hemiplegic. Certainly Jessica had PTSD from the surgeries and hospitalizations. I am hesitant to work with people on medication due to the interfering emotional blunting, but upon hearing mom’s story, I agreed.
I found Jessica to be delightful, ready and not only willing, but eager to do the deep work in her Personal Intensive. A psychology major in college, Jessica had interesting insights, and I trusted her observations about her recent hospitalization, such as being medicated more and told not to cry in her hospital room, which just made her feel worse. Jessica said that although sometimes sad or angry, she had never felt suicidal before; she woke up feeling badly depressed and thought killing herself was “a good thing to do.” She explained that the second “attempt”, while hospitalized, was a call for further help. Jessica laughed that if she really wanted to kill herself she would not try it in the hospital.
Jessica began Cymbalta ten days before the first attempt. She had told her family physician she was stressed out from school pressures and a relationship turned sour. (Typical college student stressors.) There was no time taken or simple counseling by the physician, nor suggestion to seek therapy. Just “take this drug…it will help.” As I got to know Jessica better and saw her medication history, I suspected that the psychotropic medication prescribed just before her suicide attempt may have something to do with the attempt itself; as it seemed completely out of character for this young woman, both as mom described her, and as I encountered her. Jessica said she did not want to be on any psychiatric medications.
 Research led me to psychiatrist Peter Breggin. I started with Your Drug May be Your Problem, Revised Edition: How & Why to Stop Taking Psychiatric Medications (by Peter Breggin, MD and David Cohen, PhD), which I recommended to Jessica’s parents. Further reading of Dr Breggin’s accounts of his many legal consultation clients doing bizarre things influenced by prescribed psychotropic medications (as well as numerous courts agreeing with his findings and awarding some publicized but most unpublicized hefty payments for damages by the pharmaceutical companies), it seemed more likely that Jessica’s suicide attempt was related to the psychotropic medication. I knew we had to have assistance in weaning her off and started seeking competent medical help.
Research led me to psychiatrist Peter Breggin. I started with Your Drug May be Your Problem, Revised Edition: How & Why to Stop Taking Psychiatric Medications (by Peter Breggin, MD and David Cohen, PhD), which I recommended to Jessica’s parents. Further reading of Dr Breggin’s accounts of his many legal consultation clients doing bizarre things influenced by prescribed psychotropic medications (as well as numerous courts agreeing with his findings and awarding some publicized but most unpublicized hefty payments for damages by the pharmaceutical companies), it seemed more likely that Jessica’s suicide attempt was related to the psychotropic medication. I knew we had to have assistance in weaning her off and started seeking competent medical help.
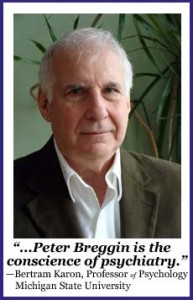
Peter Breggin MD is lauded by many of his peers in a 444-page book, The Conscience of Psychiatry: The Reform Work of Peter R. Breggin, MD. Breggin has written extensively about psychotropics’ failure to do what their developers and manufacturers claim, and how they can and sometimes do cause great harm, even when taken short-term. The pressure to medicate which parents, in particular, hear regarding their child’s inconvenient, “problematic” behaviors: “There’s no harm in giving medication a try” is false!
Jessica is now nearly weaned off Cymbalta with my support and the assistance of a caring, knowledgeable psychiatrist. She looks great and has more energy to put toward her very creative nature. Of course she still works to resolve the PTSD from her many surgeries and hospitalizations. And with fewer drugs in her system she is much better able to actively participate in, and handle, her healing work. Daily diligent work such as physical grounding and learning to deal with feelings is needed but Jessica reports feeling better than ever and continues to prefer feeling self-empowered.
Case 3: A few months ago, Marta, an intelligent woman with a young child, came to me for Intensive psychotherapy, saying she really needed help. Her family as she described it is extremely controlling and that was no longer acceptable to her. Within our first couple of hours together she told me that she had been prescribed 4 psychiatric medications by a psychiatrist – “Mother’s friend” – when Marta’s mother had called him and said her daughter was acting “crazy” and needed to be medicated. Marta told me she had been on these medications for over 5 years, and did not want to be on any! She had already begun to decrease them on her own. While medicated Marta could see some of the harm her family was creating in her life but she did not have the energy or proper brain function to change much. Marta said she had asked her physician several times, but he never explained her diagnoses or why he was prescribing the drugs. It seemed clear to me that Marta’s mother, perhaps unconsciously, wanted to control her and medications were a way to do that.
It may seem shocking that a physician would go along with this but after much research I now know that doctors, including psychiatrists can also be taken in by Big Pharma’s advertising and other motivating techniques, which strongly encourage the writing of prescriptions.
As Marta is weaning off the medications she can recognize more clearly what is happening and has more ability to be her own person. She feels quite a bit better now, three months into her slow weaning process.
Psychiatrists originally were psychoanalysts or psychotherapists, spending time and listening to clients, but now most are trained virtually all in chemical medicine and the prescription of such drugs. They typically spend an average of 13 minutes with each patient, partially due to insurance guidelines. Counselors, psychotherapists, and social workers are often partially trained, influenced and sometimes employed by psychiatrists who are often paid by pharmaceutical companies to give Continuing Education trainings about psychiatric medications.
We psychotherapists have become afraid not to refer for medications; our basic education does not train us to practice in-depth psychotherapy, or how to be most helpful with issues of real trauma. Again perhaps because of insurance guidelines we feel we cannot take the time to sit and listen for the lengthy periods needed to best help someone in distress.
We have been taught to be afraid. What if we shifted that paradigm radically:
“Emotional suffering is inevitable in life. But it has meaning – a purpose. Suffering is a signal that life matters. Specifically, it is usually a signal that something in our lives that matters a great deal needs to be addressed. Depression, guilt, anxiety, shame, chronic anger, emotional numbing – all of these reactions signal that something is amiss and requires special attention. The depth of suffering is a sign of the soul’s desire for a better, more creative, more principled life.” (Your Drug May Be Your Problem, Revised Edition: How & Why to Stop Taking Psychiatric Medications by Peter R Breggin, MD & David Cohen, PhD, 2007, pg 21).
Another recent experience bears telling. Randy became ill and was diagnosed with Adrenal Fatigue – symptoms included high anxiety due to cortisol being dumped into his system at seemingly random times.
It is now clear that his illness erupted 45 years after a six month suppression of a huge emotional outburst at age 16. A good kid, into sports and doing well in school, but the son of an alcoholic father and a very shaming, demanding mother – suddenly Randy started crying all day, every day. Hospitalized for a week, he was given drugs to “calm him down” and to help him sleep. He basically slept through the next six months.
No real psychotherapy was pursued and the family never discussed his experience. Similar to Angie’s experience, his bodymind eventually could no longer hold the emotion and it came out as a physical illness. Now he knows he learned to repress his feelings and is in process of going back to express the emotions that were blocked by medicating him into a zombie-like sleep state as a teenager – especially problematic during vital years of brain and self-image development.
It is clear that we need more training to deal with the thousands of people who have had trauma and have overwhelming feelings that must be expressed with professionals who are not frightened by strong feelings. Good therapy takes more than being OK with feelings; we also need to understand developmental stages and challenges, and how to more effectively support and empower someone to truly heal. We need to be versed in the art of being grounded, expansive helpers to support each individual to find their truth and vital health. Let’s go get that training. Possibilities for training include Dr Peter Levine, USABP (United States Association for Body Psychotherapy), David Bercelli PhD, Bioenergetics Analysis, Vitally Alive Core Energetics Institute, Psychosynthesis, among others. We must also be vigilant and do our own therapy so we may stay clear of the countertransference traps that scare us into hair-trigger medication madness …that has us referring clients for questionable medication.
[Author’s Note: I am aware that even discussing psychiatric medication with professionals evokes controversy, to the point of eliciting strong emotions. I do not work in a medical facility nor work with seriously mentally ill patients in my practice. I realize that many of you have different work experiences than mine and will have differing opinions about medications. My hopes are that my case experiences and references will inspire you to learn more, and to open a dialogue among us that needs to occur. (PLC)]
Recommended References/Resources:
Unstuck: Your Guide to the Seven-Stage Journey Out of Depression by James S. Gordon, MD (2008)
Your Drug May Be Your Problem, Revised Edition: How & Why to Stop Taking Psychiatric Medications by Peter Breggin, MD & David Cohen, PhD (2007)
Medication Madness: A Psychiatrist Exposes the Dangers of Mood-Altering Medications by Peter Breggin, MD (2008)
Psychiatric Drug Withdrawal: A Guide for Prescribers, Therapists & Their Families by Peter Breggin MD (2013)
Anatomy of an Epidemic: Magic Bullets, Psychiatric Drugs, and the Astonishing Rise of Mental Illness in America by Robert Whitaker (2011)
Not Crazy: You May Not be Mentally Ill by Charles Whitfield, MD (2011)
Ritalin is Not The Answer: A Drug Free, Practical Program for Children Diagnosed with ADD or ADHD by David B. Stein, PhD (1999)
Dosed: The Medication Generation Grows Up by Kaitlin Bell Barnett (2012)**
The Trauma Spectrum: Hidden Wounds and Human Resiliency by Robert Scaer, MD (2005)
Somatic Experiencing: The Trauma Institute www.TraumaHealing.com
Center for the Study of Empathic Therapy, Education & Living www.EmpathicTherapy.org
Vitally Alive Core Energetics Institute South www.VitallyAlive.com
United States Association for Body Psychotherapy www.USABP.org **
”In one of the most egregious examples of fraudulent marketing, ‘In the case of Paxil, prosecutors claim GlaxoSmithKline employed several tactics aimed at promoting the use of the drug in children, including helping to publish a medical journal article that misreported data from a clinical trial,’ [according to The New York Times].”

Great content! Keep up the good work!